Navigating Slipped Disc Sciatica: Symptoms, Diagnosis, and Treatment Options
Have you ever felt a sharp, shooting pain that seems to travel from your lower back down your legs? If so, you might be dealing with slipped disc sciatica. This condition, often misunderstood, can drastically affect daily life. It's more than just a backache; it's a problem that involves nerve irritation stemming from sciatica from disc herniation. This happens when a disc in your spine bulges or ruptures, pressing on nerves and causing intense pain.
The significance of understanding sciatica disc prolapse can't be overstated. With proper diagnosis and a sciatica herniated disc MRI, individuals suffering from disc prolapse sciatica can find a path to relief. Knowing the symptoms and seeking the right treatment options is key to regaining comfort and mobility. This post will guide you through the intricacies of this condition, offering insights into effective management strategies. Stay engaged; your journey to understanding begins here.
Understanding Slipped Disc Sciatica
Slipped disc sciatica is a condition that affects the spine, often leading to debilitating pain and discomfort. Understanding how your spine functions can help you see why a slipped disc can create such intense symptoms.
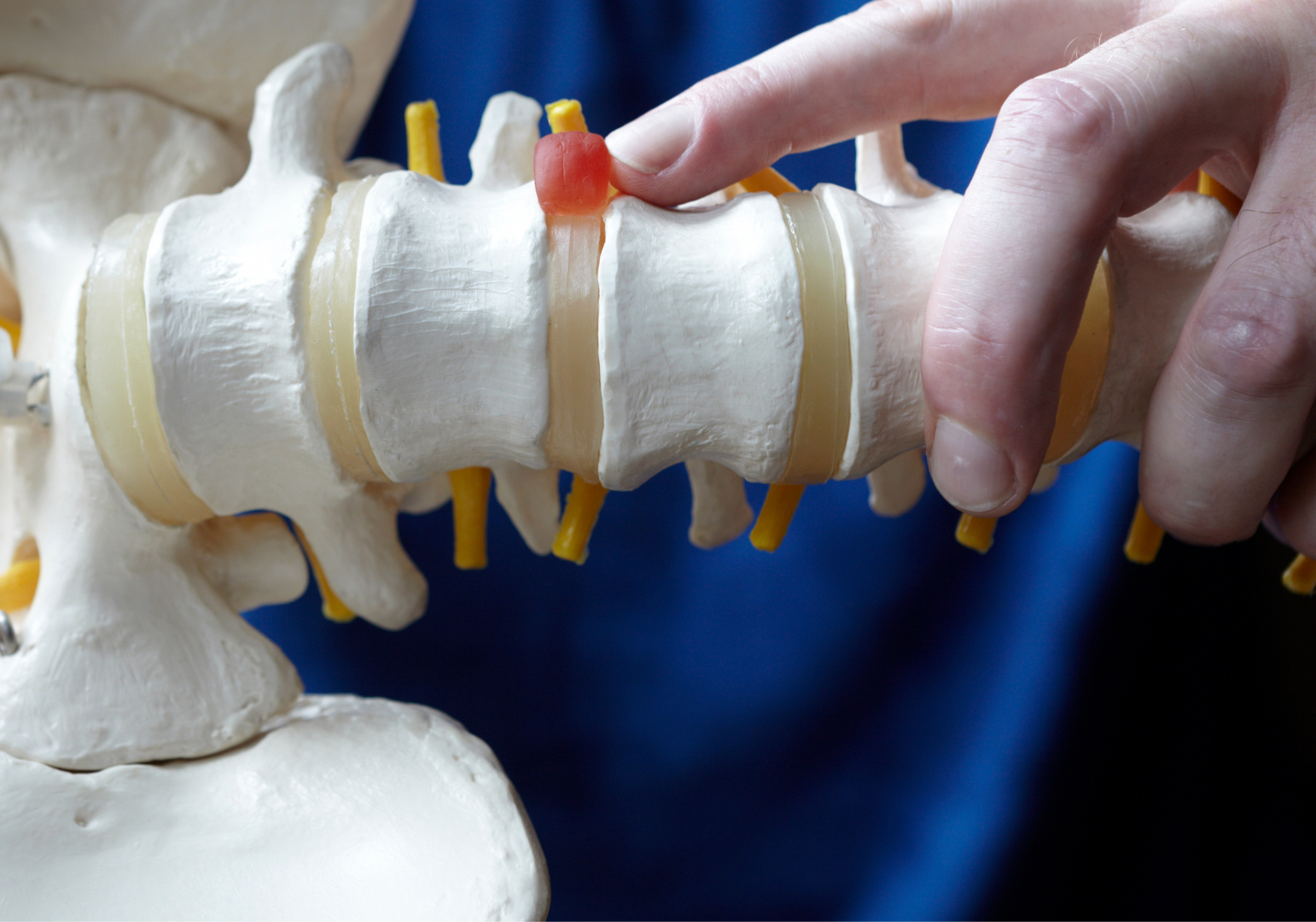
Overview of the Spine and Discs
Your spine is the backbone of your body, literally and figuratively. It’s a complex structure composed of vertebrae stacked on top of each other. The vertebrae are like the building blocks of the spine, giving it structure and protection while allowing for flexibility. Between these vertebrae are intervertebral discs, which function much like shock absorbers separating the bones. These discs have a tough outer layer and a gel-like center. They cushion the spine and allow for movement.
When these discs are healthy, they act like a cushiony doughnut, keeping the gel nicely in place. But when they’re compromised, things can go awry, leading us to our next sub-section.
Mechanism of Injury
A slipped disc, also known as a herniated disc, occurs when the inner gel of a disc bulges out through the outer layer. This can happen due to wear and tear over time or a sudden injury. The discs may shift or rupture, pressing on nearby nerves, and this is where sciatica from disc herniation comes into play.
When the herniation happens in the lower back, it can compress the large sciatic nerve, leading to disc prolapse sciatica. This pressure on the nerve causes the characteristic shooting pain and discomfort known as sciatica disc prolapse.
Symptoms vary but often include:
- Sharp pain radiating from the lower back down through the buttocks and legs.
- Numbness along the nerve pathway.
- Tingling sensations or a pins-and-needles feeling.
For precise diagnosis, many rely on a sciatica herniated disc MRI, which offers a detailed look inside the spine. With clear imaging, doctors can see the full extent of the herniation, making it possible to plan effective treatment. This level of insight is crucial for addressing not just the symptoms but the root cause of the problem.
Understanding the mechanics behind a slipped disc and its impact on nerve function helps demystify the searing pain often associated with sciatica due to disc herniation.
Symptoms of Slipped Disc Sciatica
Understanding the symptoms of slipped disc sciatica is crucial for anyone who has experienced the discomfort of nerve pain cascading from the lower back into the leg. This condition can wholly disrupt daily routines and quality of life. Recognizing these symptoms early can lead to more effective management and a quicker path to relief.
Pain Characteristics
The primary pain characteristic of sciatica from disc herniation is a sharp, shooting pain that originates in the lower back and radiates down one leg. This pain can feel like an electrifying jolt that comes and goes, often triggered by specific movements or positions. People describe this sensation as debilitating, sometimes preventing simple tasks like standing or walking. The pain typically follows a path stretching from the back, along the buttock, and down the back of the leg.
Numbness and Weakness
Another telltale sign of disc prolapse sciatica is the sensation of numbness or weakness in the affected leg. This occurs when the herniated disc compresses the sciatic nerve. You may notice numb patches or a pins-and-needles feeling that makes the leg seem disconnected from the rest of the body. In severe cases, this nerve pressure can lead to muscle weakness, impacting your ability to lift the foot or point your toes—an indicator of significant nerve involvement.
Aggravating Factors
Certain activities and positions can exacerbate sciatica disc prolapse, making symptoms more intense. Here are some common aggravating factors to watch for:
- Sitting for long periods: Prolonged sitting, especially in uncomfortable chairs, can increase pressure on the lower spine.
- Bending or lifting: Activities that involve bending forward or lifting heavy objects might trigger or worsen symptoms.
- Twisting the spine: Quick or awkward twisting motions can irritate the nerve further.
Understanding these aggravating factors helps in avoiding or modifying certain behaviors to lessen the strain on your spine, leading to better management of slipped disc sciatica symptoms. Recognizing and adjusting activities that trigger pain is a vital step towards finding relief.
Diagnosis of Slipped Disc Sciatica
When you're suffering from the nagging pain of slipped disc sciatica, getting a precise diagnosis is the first step towards relief. Accurate diagnosis ensures that the treatment plan is tailored to alleviate the distinct symptoms caused by sciatica from disc herniation. Here's how this process unfolds.
Medical History and Physical Examination
The journey to diagnosing disc prolapse sciatica begins with a thorough medical history and physical examination. Your doctor will start by asking about the nature of your pain, its duration, and any accompanying symptoms. Important details include the pain's severity, its specific location, and any factors that worsen or relieve it.
During the physical examination, the doctor assesses your spine for signs of tenderness, muscle weakness, and reflex issues. They might test your sensory responses to pinpoint the nerves involved. This initial evaluation helps rule out other potential causes of back pain, steering the diagnosis towards sciatica disc prolapse.
Imaging Techniques
For a deeper look, imaging techniques come into play, particularly the use of MRI (Magnetic Resonance Imaging). An MRI is pivotal in diagnosing a sciatica herniated disc. It provides a detailed image of your spine’s soft tissues, unlike X-rays that focus primarily on bones. This clarity allows doctors to see the herniation and assess how it's compressing the sciatic nerve.
MRI scans are crucial because they not only confirm the presence of a herniated disc but also measure its size and exact location. This information is essential in tailoring treatments to address the specific aspects of the disc herniation causing your symptoms.
Differential Diagnosis
Diagnosis isn’t just about pinpointing the obvious; it also involves eliminating other conditions that mimic slipped disc sciatica. Some conditions have similar symptoms, such as:
- Piriformis Syndrome: This condition can irritate the sciatic nerve similarly, but the cause is a muscle in the buttock area.
- Spinal Stenosis: Involves narrowing of the spinal canal and can cause nerve compression, leading to pain.
- Degenerative Disc Disease: Often confuses because it causes similar nerve pain symptoms but arises from wear and tear over time.
Differential diagnosis is critical to avoid unsuccessful treatments by addressing the wrong condition. A thorough evaluation combining medical history, physical examination, and imaging tests ensures that the diagnosis is accurate and individualized treatment plans are effective. Your understanding of the diagnosis process can empower you to make informed decisions, guiding your path to recovery.
Treatment Options for Slipped Disc Sciatica
When it comes to managing the discomfort of slipped disc sciatica, understanding the variety of treatment options can open the door to relief. These options range from conservative approaches to surgical interventions, each tailored to suit different levels of severity and individual needs. Navigating these choices can be daunting, but with the right information, you can find a path that works for you.
Conservative Treatments
For many experiencing sciatica from disc herniation, conservative treatments offer a first line of defense. These methods focus on alleviating pain and improving mobility through non-invasive techniques.

- Physical Therapy: Engaging in targeted exercises can strengthen back muscles, which helps support the spine and alleviate pressure on the discs. Physical therapists might suggest a series of stretches and strength-building routines tailored to your condition.
- Medications: Over-the-counter pain relievers, like ibuprofen or acetaminophen, can reduce inflammation and ease discomfort. In some cases, doctors might prescribe muscle relaxants or stronger pain medications.
- Lifestyle Modifications: Simple changes can make a big difference. Maintaining a healthy weight, staying active with low-impact exercises like swimming or walking, and avoiding prolonged sitting can reduce stress on the spine.
Surgical Interventions
While many find relief with conservative methods, others might need to consider surgical options, particularly when symptoms persist or worsen.
Surgery is typically indicated when:
- There's significant pain that does not improve with other treatments.
- Neurological deficits, such as weakness, persist or worsen.
- Loss of bowel or bladder control occurs.
The types of surgical procedures available include:
- Microdiscectomy: This minimally invasive procedure involves removing the herniated portion of the disc to relieve nerve pressure.
- Laminectomy: This surgery removes part of the vertebra known as the lamina to create more space for the spinal nerves, often addressing spinal stenosis that's caused by disc prolapse sciatica.
Rehabilitation and Recovery
Post-treatment rehabilitation is crucial for regaining full function and managing sciatica disc prolapse symptoms. An effective rehab program focuses on:
- Strengthening Muscles: Building core and spine-supporting muscles to prevent future injuries.
- Flexibility Exercises: Stretching routines to maintain mobility and lessen nerve compression.
- Education: Learning proper techniques for lifting and posture to avoid recurrent slipped disc sciatica issues.
Rehab isn't just about physical healing; it's a journey towards reclaiming your life free from the debilitating effects of sciatica herniated disc MRI findings. Understanding your treatment options and working closely with healthcare professionals can pave the way for a balanced, less painful life.
Preventing Slipped Disc Sciatica
Slipped disc sciatica is not only painful but can also be a significant hindrance in daily life. Prevention plays a crucial role. By adopting correct habits and techniques, you can protect your spine and reduce the risk of sciatica from disc herniation. Let's explore some effective strategies.
Proper Lifting Techniques
Improper lifting can place excessive stress on your spine, leading to slipped disc sciatica. How you lift objects, whether heavy or light, makes a significant difference. Picture your spine as a stack of delicate china plates; one wrong move, and there's a risk of toppling them over. That's why using proper lifting techniques is so imperative.
1. Bend your knees, not your waist: This basic rule shifts the weight from your back to your legs, which are better equipped to handle the load.
2. Keep the object close: Maintain the object you're lifting close to your body. This reduces the strain on your lower back.
3. Use your legs: Your legs are powerhouses. Let them do the heavy lifting, literally.
4. Avoid twisting: Twisting while lifting can stress your spine. Instead, pivot your feet to turn.
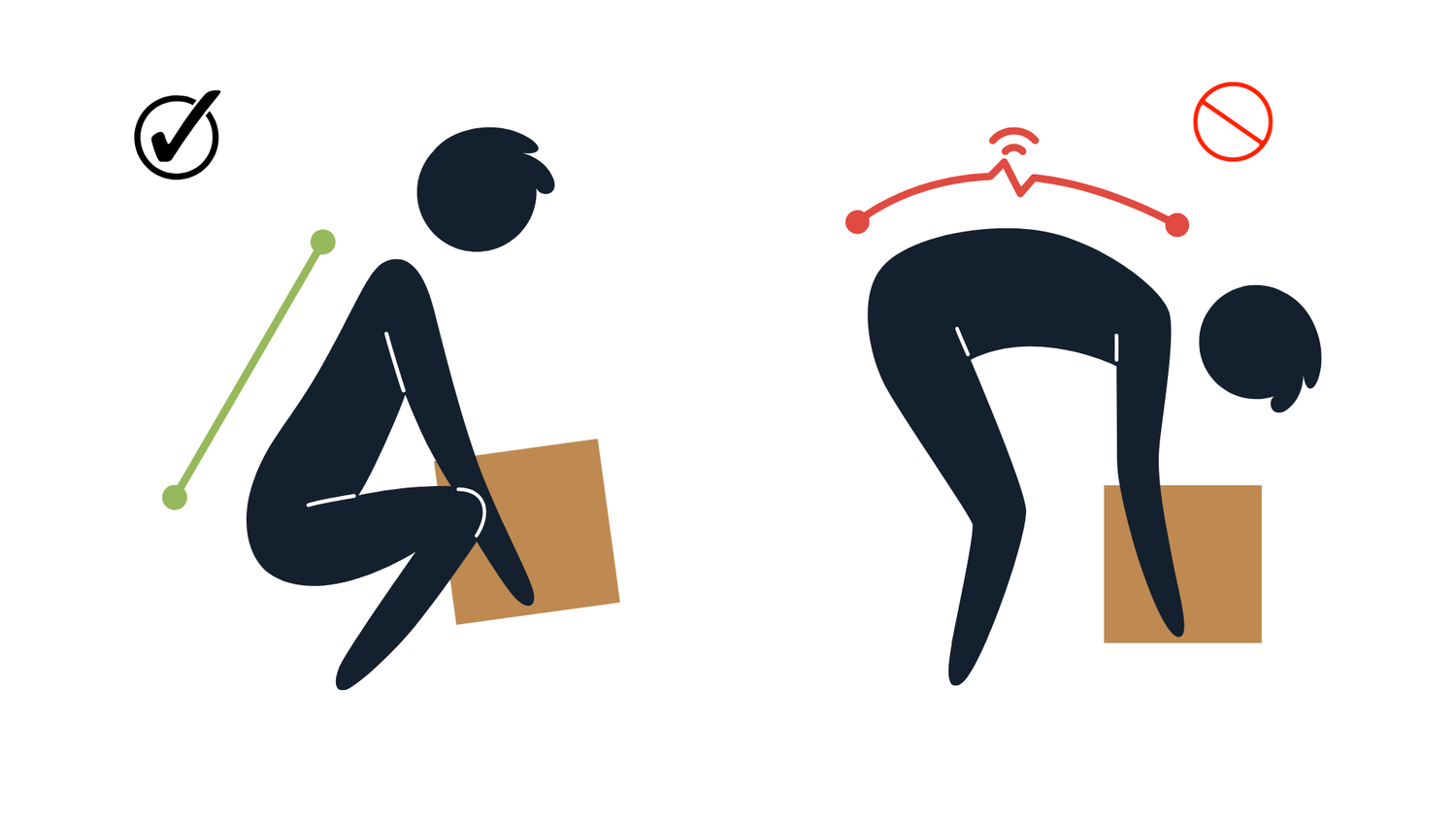
Mastering these techniques can lessen the burden on your spine, ensuring you’re less likely to suffer from sciatica disc prolapse.
Exercise and Strength Training
Exercise isn't just a way to stay fit; it's your spine's best friend. Regular physical activity strengthens the muscles supporting your spine, reduces sciatica symptoms, and helps prevent disc prolapse sciatica.
- Core Strengthening: A strong core is a spine’s stable base. Exercises like planks and bridges build core muscles, reducing the likelihood of a slipped disc.
- Flexibility Exercises: Stretching, such as yoga or Pilates, enhances flexibility, reducing the risk of disc issues. They nurture a more supple spine and help prevent rigidity, which can lead to injuries.
- Low-impact Aerobics: Activities like swimming or cycling improve cardiovascular health without jarring your spine.

Through consistent exercise, you not only build strength but also equip your body to better handle physical stresses, decreasing the risk of sciatica herniated disc complications. Remember, an active body is a resilient body.
Living with Slipped Disc Sciatica
Living with slipped disc sciatica can be challenging, as it often disrupts day-to-day activities with persistent discomfort and pain. Finding ways to manage this condition is essential for improving quality of life and maintaining independence. Here's how to adapt daily activities to minimize strain on your back and where to seek the necessary support.
Adapting Daily Activities
Adapting how we approach everyday tasks can significantly reduce back strain, especially when living with sciatica from disc herniation. Your spine is like a finely tuned instrument that requires careful handling to keep it in harmony. Here's how you can tweak daily activities to support your spine:
- Mindful Movement: Use your legs as levers when lifting objects by bending at the knees instead of the waist. This technique keeps your back straight and minimizes pressure.
- Ergonomic Adjustments: Set up an ergonomic workspace. Ensure chairs and desks are at the correct heights to maintain a neutral spine position. Using a lumbar cushion can add extra support.
- Frequent Breaks: Whether working at a desk or doing household chores, take regular breaks to stretch and relax your muscles. Gentle stretching can alleviate tension and prevent stiffness.
- Footwear Considerations: Choose supportive shoes with low heels. High heels can shift body weight forward, straining your back.
Small adjustments in daily routines can have a big impact on managing disc prolapse sciatica symptoms.
Support Systems
Engaging support systems is crucial in navigating sciatica disc prolapse. Embracing support from healthcare providers and community resources can provide the guidance and encouragement needed to manage this condition effectively.
- Healthcare Providers: A multidisciplinary approach involving doctors, physical therapists, and chiropractors can tailor a management plan to your specific needs. Regular consultations and follow-ups ensure you stay on track.
- Community Support: Joining support groups or forums offers emotional backing and practical advice from others who understand your journey. Sharing experiences can be comforting and empowering.
- Mental Health Resources: Chronic pain can take a toll on mental health. Consider speaking with a counselor or therapist to address any emotional challenges associated with living with sciatica herniated disc MRI findings.
Connecting with these support systems can ease the strain and foster resilience, making it easier to manage slipped disc sciatica effectively.
Conclusion
Slipped disc sciatica can significantly impact daily life. The sharp pain and discomfort of sciatica from disc herniation requires attention and care. Recognizing symptoms like numbness or shooting pain can lead to quicker diagnosis and treatment. Through a sciatica herniated disc MRI, healthcare providers can create personalized treatment plans. Understanding this condition and implementing prevention strategies are crucial for managing disc prolapse sciatica.
Whether using conservative treatments or considering surgery, understanding your options is key. Committing to proper lifting techniques and maintaining an active lifestyle can help prevent sciatica disc prolapse. Engage with healthcare professionals and support networks to navigate this challenging condition. How has your experience with slipped disc sciatica shaped your approach to care and prevention? Share your thoughts and take control of your spinal health.

You Can Fix Your Back...
You Just Need The Right Program
- Reduce your sciatic pain in days, not weeks.
- No more endless doctor visits—take control at home.
- Empower yourself with a program backed by real results.
- 2024 Sciatica Self Treatment / Back Pain Self Treatment














